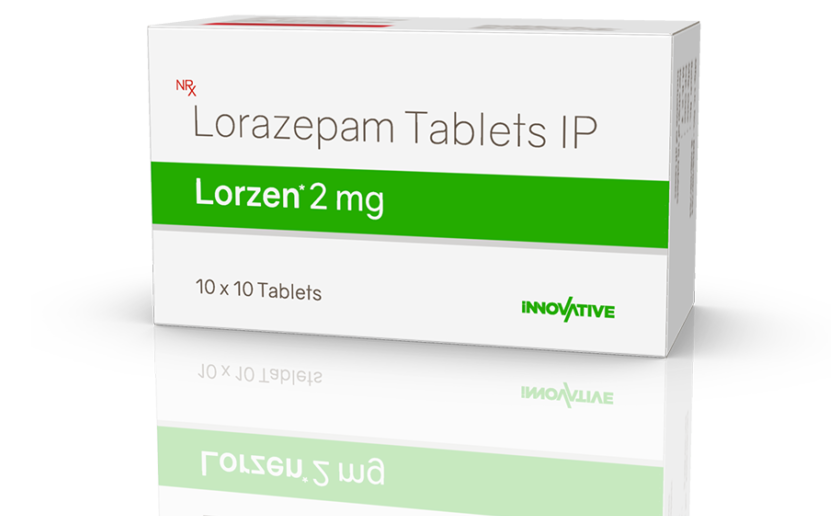
Lorazepam 2mg: Uses, Benefits, and Precautions
Mechanism of Action
GABA Receptor Interaction
- Reduced neuron excitability
- Decreased anxiety and tension
- Promotion of relaxation and sleep
Rapid Onset of Action
Duration of Effects
Regular use of lorazepam may lead to tolerance, requiring higher doses for the same effect. Physical dependence can also develop, so discontinuation should be managed carefully with gradual dose reduction.
Medical Uses and Indications
Anxiety Disorders
- Generalised Anxiety Disorder (GAD)
- Panic Disorder
- Social Anxiety Disorder
- Specific Phobias
- Reduce the time it takes to fall asleep
- Increase total sleep time
- Improve sleep quality
Pre-operative Sedation
- Reduce anxiety related to upcoming procedures
- Induce amnesia, preventing recall of potentially distressing events
- Enhance the effects of anaesthesia
Under medical supervision, lorazepam may be used to manage symptoms of acute alcohol withdrawal syndrome. It is effective in preventing or treating:
- Seizures
- Delirium tremens
- Severe anxiety and agitation
Chemotherapy-induced Nausea
Epilepsy
Off-label Uses
- Vertigo and dizziness
- Tension headaches
- Irritable bowel syndrome (IBS)
Dosage and Administration
Standard Dosing Guidelines
- Anxiety disorders: 2-3 mg/day, divided into 2-3 doses
- Insomnia: 2-4 mg at bedtime
- Pre-operative sedation: 2-4 mg the night before surgery
Administration Methods
- Tablets: The most common form, taken orally with or without food
- Sublingual tablets: Placed under the tongue for faster absorption
- Oral concentrate: A liquid form that can be mixed with liquids or semi-solid foods
- Injectable solution: For hospital use in emergencies or severe cases
Timing Considerations
- For anxiety: Doses are typically spread throughout the day, with the last dose often taken at bedtime
- For insomnia: Taken 30-60 minutes before desired sleep time
- For pre-operative use: Usually given 1-2 hours before the procedure
Duration of Treatment
Special Populations
- Elderly patients: Often start with half the standard adult dose due to increased sensitivity
- Patients with liver impairment: May require lower doses or extended intervals between doses
- Individuals with respiratory conditions: Careful monitoring is necessary due to the potential for respiratory depression
Missed Doses
Discontinuation
Side Effects and Adverse Reactions
Common Side Effects
- Drowsiness and sedation
- Dizziness
- Weakness or unsteadiness
- Blurred vision
- Dry mouth
- Nausea or changes in appetite
- Headache
- Confusion or disorientation
Cognitive and Psychomotor Effects
- Decreased concentration and attention span
- Impaired memory, particularly short-term recall
- Slowed reaction times
- Reduced coordination
Paradoxical Reactions
- Increased anxiety or agitation
- Aggression or hostility
- Hallucinations
- Insomnia
Respiratory Depression
Allergic Reactions
- Skin rashes or hives
- Itching
- Swelling of the face, lips, tongue, or throat
- Difficulty breathing
Long-term Effects
- Tolerance: Requiring higher doses to achieve the same therapeutic effect
- Dependence: Physical and psychological reliance on the medication
- Cognitive decline: Potential impact on memory and cognitive function, especially in elderly patients
- Increased risk of falls and fractures in older adults
Withdrawal Symptoms
- Rebound anxiety or insomnia
- Irritability and restlessness
- Tremors
- Sweating
- Nausea and vomiting
- In severe cases, seizures or hallucinations
Rare but Serious Adverse Effects
- Severe skin reactions (e.g., Stevens-Johnson syndrome)
- Liver dysfunction
- Blood disorders
- Suicidal thoughts or behaviors (particularly in patients with depression)
Monitoring and Reporting
Central Nervous System (CNS) Depressants
- Opioid pain medications (e.g., morphine, oxycodone)
- Alcohol
- Barbiturates
- Other benzodiazepines
- Certain antidepressants
- Antihistamines with sedating properties
Antidepressants
- SSRIs: Generally safe, but may increase sedation
- MAOIs: Can potentiate the effects of lorazepam
- Tricyclic antidepressants: May increase sedation and anticholinergic effects
Anticonvulsants
- Carbamazepine: May decrease lorazepam levels
- Valproic acid: Can increase lorazepam concentrations
Antipsychotics
Probenecid
Theophylline
Caffeine
Herbal Supplements
- St. John’s Wort: May decrease lorazepam levels
- Valerian root: Can increase sedation
- Kava kava: May enhance CNS depression
Grapefruit Juice
Contraceptives
Digoxin
Anesthetics
Management of Drug Interactions
- Maintain an up-to-date list of all medications and supplements
- Inform all healthcare providers about lorazepam use
- Avoid alcohol consumption while taking lorazepam
- Do not start or stop any medications without consulting a healthcare provider
- Be aware of potential interactions with over-the-counter products
Contraindications and Precautions
Absolute Contraindications
- Known hypersensitivity to lorazepam or other benzodiazepines
- Acute narrow-angle glaucoma
- Myasthenia gravis (a neuromuscular disorder)
- Severe respiratory insufficiency
- Sleep apnea syndrome
Relative Contraindications
- Chronic respiratory diseases (e.g., COPD, asthma)
- Liver or kidney impairment
- History of substance abuse or addiction
- Severe depression or suicidal tendencies
- Personality disorders
- Acute alcohol intoxication
Pregnancy and Breastfeeding
Pediatric Use
Geriatric Use
- Increased risk of falls and fractures
- Potential for cognitive impairment
- Greater susceptibility to respiratory depression
Occupational Hazards
History of Seizures
Psychiatric Conditions
- Bipolar disorder
- Schizophrenia
- Personality disorders
Hepatic Impairment
Renal Impairment
History of Substance Abuse
Precautions During Long-term Use
- Regular reassessment of the need for continued therapy
- Monitoring for development of tolerance or dependence
- Periodic liver and kidney function tests
- Assessment of cognitive function, especially in older adults
Discontinuation Precautions
- Gradual tapering of the dose is essential to minimise withdrawal symptoms.
- Close medical supervision during the tapering process
- Consideration of alternative treatments or coping strategies for the underlying anxiety
Pharmacokinetics and Metabolism
Absorption
- Peak plasma concentrations are reached within 1-2 hours after oral administration
- The presence of food in the stomach does not significantly affect absorption
- Sublingual administration can lead to a faster onset of action
Distribution
- It readily crosses the blood-brain barrier due to its lipophilic nature
- Approximately 85% of lorazepam in the bloodstream is bound to plasma proteins
- The volume of distribution is relatively small, indicating limited tissue distribution
Metabolism
- The main metabolic pathway involves conjugation with glucuronic acid
- This process forms an inactive metabolite, lorazepam glucuronide
- Unlike some other benzodiazepines, lorazepam does not undergo significant oxidative metabolism via the cytochrome P450 system
Elimination
- The elimination half-life of lorazepam is approximately 12-18 hours in healthy adults
- Lorazepam glucuronide is excreted in the urine
- A small amount of unchanged lorazepam may also be excreted in the urine
Factors Affecting Pharmacokinetics
- Age: Elderly patients may have prolonged elimination half-lives
- Liver function: Impaired hepatic function can lead to decreased metabolism and increased drug accumulation
- Kidney function: Severe renal impairment may affect the excretion of lorazepam glucuronide
- Body composition: Obesity can increase the volume of distribution and potentially prolong the effects
- Genetic factors: Variations in glucuronidation enzymes may affect metabolism rates
Steady-State Concentrations
Comparison to Other Benzodiazepines
- No active metabolites, leading to more predictable effects
- Less accumulation in patients with liver disease due to the liver’s glucuronidation pathway
- Relatively long half-life compared to short-acting benzodiazepines, allowing for less frequent dosing
Implications for Clinical Use
- Dosing frequency: Typically 2-3 times daily for anxiety management
- Onset of action: Rapid effects make it suitable for acute anxiety relief
- Duration of action: Intermediate duration allows for sustained anxiolytic effects
- Potential for accumulation: Consideration in patients with impaired metabolism or elimination
Drug Interactions Based on Metabolism
- Probenecid: Can inhibit glucuronidation, potentially increasing lorazepam levels
- Valproic acid: May compete for glucuronidation enzymes, affecting lorazepam metabolism
Therapeutic Drug Monitoring
- Suspected toxicity or overdose
- Assessing adherence in some clinical settings
- Managing complex drug interactions
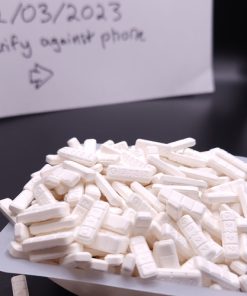
Safety and Overdose Considerations
Signs of Overdose
- Extreme drowsiness or difficulty staying awake
- Confusion or disorientation
- Slurred speech
- Impaired coordination and balance
- Slow or shallow breathing
- Weak pulse
- Coma (in severe cases)
Risk Factors for Overdose
- Combining lorazepam with alcohol or other CNS depressants
- History of substance abuse
- Elderly patients or those with impaired liver function
- Intentional misuse or abuse of the medication
- Accidental ingestion, particularly in children
Emergency Response to Overdose
- Call emergency services immediately
- Provide information about the amount ingested and timing if known
- Follow instructions from emergency personnel
- If the person is unconscious but breathing, place them in the recovery position
- Do not induce vomiting unless instructed by medical professionals
Medical Treatment for Overdose
- Administration of flumazenil, a benzodiazepine antagonist (used cautiously due to potential risks)
- Supportive care, including respiratory support if needed
- Monitoring of vital signs and neurological status
- Intravenous fluids and other supportive measures
Prevention of Accidental Overdose
- Store medication securely, out of reach of children and others
- Use child-resistant packaging
- Dispose of unused medication properly through drug take-back programs
- Never share prescription medication with others
- Adhere strictly to prescribed dosages and schedules
Safe Storage and Disposal
- Keep in original container at room temperature
- Store away from heat, moisture, and direct light
- Use a locked medicine cabinet if possible
- Follow local guidelines for safe disposal of unused medication
Patient Education
- Proper use and potential risks of lorazepam
- Importance of not combining with alcohol or other sedatives
- Signs of overdose and when to seek emergency care
- Safe storage and disposal practices
Monitoring and Follow-up
- Scheduled follow-up appointments to assess effectiveness and side effects
- Periodic reassessment of the need for continued treatment
- Screening for signs of dependence or misuse
Special Populations
- Elderly patients: Higher risk of falls and cognitive impairment
- Patients with respiratory conditions: Increased risk of respiratory depression
- Individuals with a history of substance abuse: Higher risk of misuse or dependence
Pregnancy and Breastfeeding Considerations
- Potential risks to the fetus or infant should be weighed against benefits
- Alternative treatments may be preferred when possible
- If used during pregnancy, neonatal monitoring may be necessary
Long-term Safety Considerations
- Regular assessment of cognitive function, especially in older adults
- Monitoring for development of tolerance or dependence
- Consideration of periodic “drug holidays” or dose reductions when appropriate
Reporting Adverse Events
Controlled Substance Classification
- It has a lower potential for abuse compared to Schedule II or III substances.
- It has accepted medical uses.
- Abuse may lead to limited physical or psychological dependence.
Prescription Requirements
- Prescriptions must meet specific legal requirements (e.g., patient information, dosage, quantity)
- Refills may be limited and subject to additional controls.
- Electronic prescribing may be mandatory in some jurisdictions to enhance security and tracking.
Dispensing Regulations
- Verification of prescription authenticity
- Maintaining detailed records of dispensed medications
- Implementing security measures to prevent theft or diversion
- Counselling patients on proper use and potential risks
International Travel Considerations
- Varying legal status in different countries
- Requirements for carrying prescription medications across borders
- Potential need for additional documentation or permits
Manufacturing and Distribution Controls
- Strict quality control standards
- Regular inspections by regulatory agencies
- Reporting requirements for production and distribution
Abuse Prevention Measures
- Prescription Drug Monitoring Programs (PDMPs) in many jurisdictions
- Limitations on quantity and duration of prescriptions
- Education programs for healthcare providers on responsible prescribing
- Public awareness campaigns about the risks of benzodiazepine misuse
Off-label Use Considerations
Generic Availability and Regulation
- Bioequivalence testing to ensure similarity to the brand-name product
- Adherence to the same quality and safety standards as brand-name medications
- Ongoing monitoring and reporting of adverse events
Special Population Considerations
- Pediatric patients
- Elderly individuals
- Pregnant women
Reporting Requirements
- Adverse drug reactions
- Quality issues with medication
- Suspected cases of abuse or diversion
Regulatory Oversight
- U.S. Food and Drug Administration (FDA)
- Drug Enforcement Administration (DEA)
- European Medicines Agency (EMA)
- World Health Organization (WHO)
Future Regulatory Trends
- Enhanced monitoring of long-term benzodiazepine use
- Stricter controls on prescribing patterns
- Increased emphasis on alternative treatments for anxiety disorders
Patient Rights and Responsibilities
- The right to informed consent regarding potential risks and benefits
- The responsibility to use the medication as prescribed and not share it with others
- Awareness of the legal and regulatory framework governing lorazepam 2mg is essential for its safe and appropriate use. Healthcare providers are responsible for remaining informed about current regulations and best practices, while patients should understand their rights and responsibilities when using this controlled medication. Adherence to these frameworks supports effective treatment of anxiety disorders and helps prevent misuse or diversion of lorazepam.
Alternatives and Complementary Therapies
Non-Benzodiazepine Medications
- Selective Serotonin Reuptake Inhibitors (SSRIs):
-
- Examples: Fluoxetine, Sertraline, Paroxetine
- Often considered a first-line treatment for long-term anxiety management.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs):
-
- Examples: Venlafaxine, Duloxetine
- Effective for both anxiety and depression
- Buspirone:
-
- Non-benzodiazepine anxiolytic
- Lower risk of dependence compared to benzodiazepines
- Beta-blockers:
-
- Examples: Propranolol, Atenolol
- Useful for managing physical symptoms of anxiety, particularly in performance situations
- Antihistamines:
-
- Examples: Hydroxyzine
- Can provide mild sedation and anxiety relief
Psychotherapy Approaches
- Cognitive Behavioural Therapy (CBT):
-
- Helps identify and change negative thought patterns
- Teaches coping strategies for managing anxiety
- Exposure Therapy:
-
- Gradually exposes individuals to anxiety-provoking situations
- Particularly effective for specific phobias and social anxiety
- Mindfulness-Based Stress Reduction (MBSR):
-
- Incorporates meditation and mindfulness techniques
- Helps reduce overall stress and anxiety levels
- Dialectical Behaviour Therapy (DBT):
-
- Combines cognitive-behavioural techniques with mindfulness
- Useful for managing intense emotions and improving interpersonal relationships
Lifestyle Modifications
- Regular exercise:
-
- Releases endorphins and reduces stress hormones
- Improves overall mood and well-being
- Proper sleep hygiene:
-
- Establishing consistent sleep patterns
- Creating a relaxing bedtime routine